Intrapancreatic accessory spleen: CT appearance and differential diagnosis
Satomi Kawamoto1 , Pamela T. Johnson1, Heather Hall2, John L. Cameron2, Ralph H. Hruban3 and Elliot K. Fishman1
(1) | The Russell H. Morgan Department of Radiology and Radiological Science, Johns Hopkins Hospital, JHOC 3235A, 601 North Caroline Street, Baltimore, MD 21287, USA |
(2) | Department of Surgery, Johns Hopkins School of Medicine, 600 N. Wolfe Street, Baltimore, MD 21287, USA |
(3) | Department of Pathology, The Sol Goldman Pancreatic Cancer Research Center, Johns Hopkins School of Medicine, 600 N. Wolfe Street, Baltimore, MD 21287, USA |
Abstract
Although autopsy studies report that the second most common site of the accessory spleen is in the tail of the pancreas, intrapancreatic accessory spleens (IPASs) are rarely recognized radiologically. With recent improvements in imaging techniques, IPASs are more commonly detected on imaging studies. IPAS can be mistaken for other type of mass-forming lesions in the tail of the pancreas, particularly an asymptomatic small neuroendocrine neoplasm. Rarely, an epidermoid cyst originating from IPAS may simulate other cystic pancreatic lesion. Accurate preoperative diagnosis would obviate unnecessary surgery. IPAS should be considered when a hypervascular mass is seen in the tail of the pancreas on CT. Typical location, similar attenuation of the lesion to the spleen on noncontrast, and postcontrast CT at different phases are helpful to make diagnosis of IPAS. In particular, characteristic heterogeneous contrast enhancement of IPAS on the arterial phase may be helpful for correct diagnosis. However, when it remains difficult to exclude the other diagnosis, 99mTc labeled heat-damaged red blood cell scintigraphy or superparamagnetic iron oxide-enhanced MRI can be used to confirm the diagnosis of IPAS.
Keywords Intrapancreatic accessory spleen – Pancreatic neuroendocrine neoplasm – CT – Contrast enhancement
Accessory spleen is a congenital abnormality consisting of normal splenic tissue in ectopic sites seen in approximately 10 to 20% of individuals [1, 2]. The most common location of an accessory spleen is the splenic hilum. The second most common site of the accessory spleen is in the tail of the pancreas. However, intrapancreatic accessory spleens (IPASs) are rarely recognized radiologically [3, 4].
With recent technical improvement of imaging studies, IPASs are more commonly detected on CT and MR imaging [3, 5, 6]. IPAS can be mistaken for other mass-forming lesions in the pancreas, particularly asymptomatic pancreatic neuroendocrine neoplasms. Despite advances in CT resolution, criteria to discriminate IPASs from small pancreatic neuroendocrine neoplasms have yet to be defined.
IPAS is usually asymptomatic and found incidentally on imaging studies, and generally does not require therapy. The challenge lies in reliably distinguishing a small enhancing intrapancreatic splenic rests from neuroendocrine neoplasm. Accurate preoperative distinction would obviate unnecessary surgery. The purpose of this article is to review the typical and atypical CT appearances in a series of patients with IPAS, and to discuss the characteristic appearance on CT and other imaging modalities that can be used to distinguish IPAS from other mass-forming lesions in the pancreas.
Embryology and incidence of IPAS
Accessory spleen is a congenital abnormality consisting of normal splenic tissue in ectopic sites. An accessory spleen arises as a result of failure of fusion of some of the multiple buds of splenic tissue in the dorsal mesogastrium during embryologic life [7]. Accessory spleens are usually single, but approximately 10% of patients with one have a second focus [1]. More than two deposits are seen infrequently [1, 2].
In autopsy studies, the second most common site of the accessory spleen is in the tail of the pancreas (Fig 1). Halpert et al. reported that 61 (16.8%) of 364 accessory spleens among 3,000 male patients in an autopsy study were located in the tail of the pancreas [1]. In the autopsy study by Wadham et al., 11% of accessory spleens in 250 patients involved the tail of the pancreas, usually within 3–4 cm of the splenic hilum [2].
Fig. 1 Illustration showing an accessory spleen seen as a nodule of splenic parenchyma embedded in the tail of pancreas.
In imaging studies, IPAS is less commonly encountered. In a retrospective review of CT examinations in 1,000 patients, Mortele et al. reported that a total of 180 accessory spleens were found in 156 patients (15.6%), and IPASs were found in 2 patients (0.2%) [4]. In this study, the most common location of accessory spleen was inferior third of the posteromedial portion of the splenic hilum, which was adjacent (lateral, posterior, and superior) to the tail of the pancreas [4].
Pathology
Microscopically, an IPAS reproduces the splenic pattern [8]. Usually, they have a well-defined fibrotic capsule which separates the surrounding normal pancreatic tissue [5, 8]. The capsule has a varying width, with septa [8]. In some of the IPAS, the capsule may be thin, incomplete, or missing, in which cases lymphoid tissue can be located outside and adjacent to the capsule [8]. When superimposed lesions, such as chronic congestion, hemosiderosis, lymphoproliferative disorder, are present within an IPAS, they usually have an identical appearance to the same lesions in the main spleen [8].
CT findings of IPAS
Size
Typically, IPAS appears as a solid enhancing mass with a smooth, round, ovoid or minimally lobulated shape within the tail of the pancreas. The reported size of IPAS of a series of seven cases was from 1.1 to 2.5 cm (average 1.5 ± 0.5 cm) [5]. Although the prior autopsy study reported that it is unusual that an accessory spleen exceeds 4 cm in diameter without enlargement of the main spleen [1], IPAS can be larger than 4 cm (Figs. 2, 3). When the spleen is involved with hematologic or other systemic disorder such as leukemia/lymphoma, passive congestion, hemosiderosis or thrombocytopenia, accessory spleens are usually also involved, and IPAS may change its size according to the main spleen [1, 8] (Fig. 4).
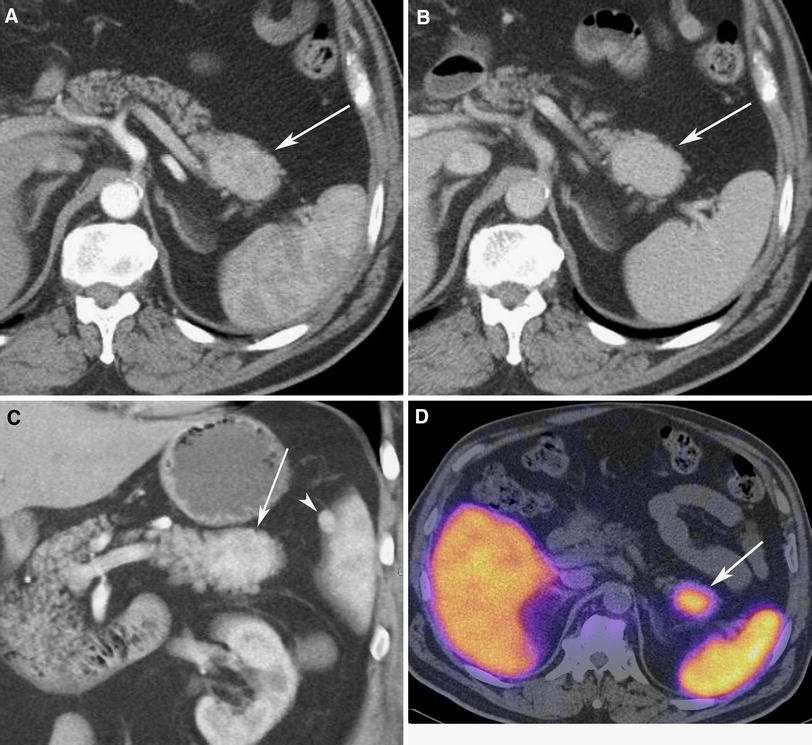
Fig. 2 66-Year-old man with history of soft tissue sarcoma. CT for staging of sarcoma showed a mass in the tail of the pancreas. A Arterial, B portal venous phase axial CT images and C arterial phase coronal volume rendered image show 4.3 × 3.5 cm enhancing solid mass in the tip of the tail of pancreas (arrow), representing intrapancreatic accessory spleen (IPAS). There is heterogeneous contrast enhancement within spleen and IPAS at arterial phase. Small additional accessory spleen is seen near the splenic hilum (arrowhead). Due to its unusually large size, Tc-99m sulfur colloid SPECT was performed. D Fused image of axial Tc-99m sulfur colloid SPECT and noncontrast CT confirmed that uptake was matched with intrapancreatic lesion on CT (arrow).
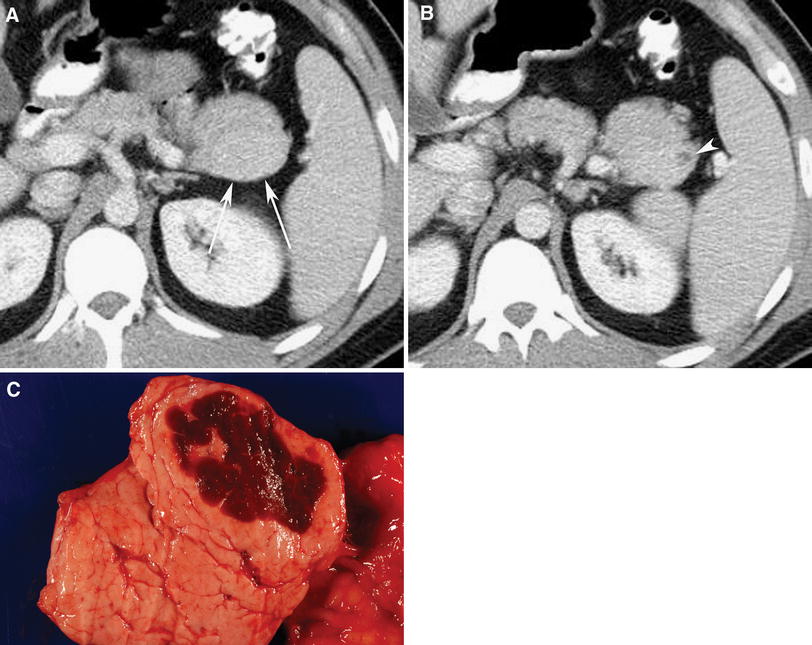
Fig. 3 27-Year-old man with history of abdominal discomfort, and mass was found in the tail of the pancreas on CT performed at another institution. A and B Venous phase axial CT images show solid mass (4.1 cm) in the tail of the pancreas, which is isodense to spleen. Small cystic component (arrowhead) is seen in periphery of mass. Neuroendocrine neoplasm was suspected, and patient underwent distal pancreatectomy and splenectomy. Pathology revealed IPAS with associated dilated pancreatic duct. C Image of gross specimen shows heterotopic spleen in tail of pancreas.
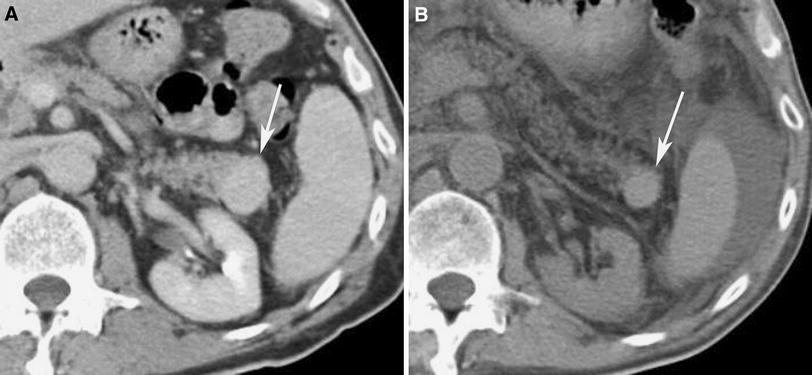
Fig. 4 60-Year-old man with history of diffuse B cell lymphoma. A Venous phase axial CT image shows solid mass (2.5 × 2.0 cm), which is isodense to spleen, in the tip of the tail of the pancreas. B Noncontrast CT obtained 11 months later (A). Patient underwent multiple chemotherapies and bone marrow transplant. Solid mass in the tail of the pancreas decreased in size (1.9 × 1.6 cm) paralleling decrease in size of the main spleen. Small amount of ascites is also seen. No histologic proof is available, but it was thought to represent IPAS.
Location
With the exception of a case reported where ectopic splenic tissue was detected within the pancreatic body after splenic injury [9], all reported IPASs have been within the tail of the pancreas. IPAS usually located at the tip of the tail of the pancreas (Figs. 2, 3, 4, 5, 6), or close to the tip of the tail of the pancreas (Figs. 7, 8). Heredia et al. reported five cases of IPAS on MRI, and they were located within 3 cm of the distal tail of the pancreas [10]. If a solid enhancing pancreatic tail mass is located more close to the body of the pancreas, it is unlikely to represent IPAS, and more likely to represent other mass such as pancreatic neuroendocrine neoplasm (Fig. 9).
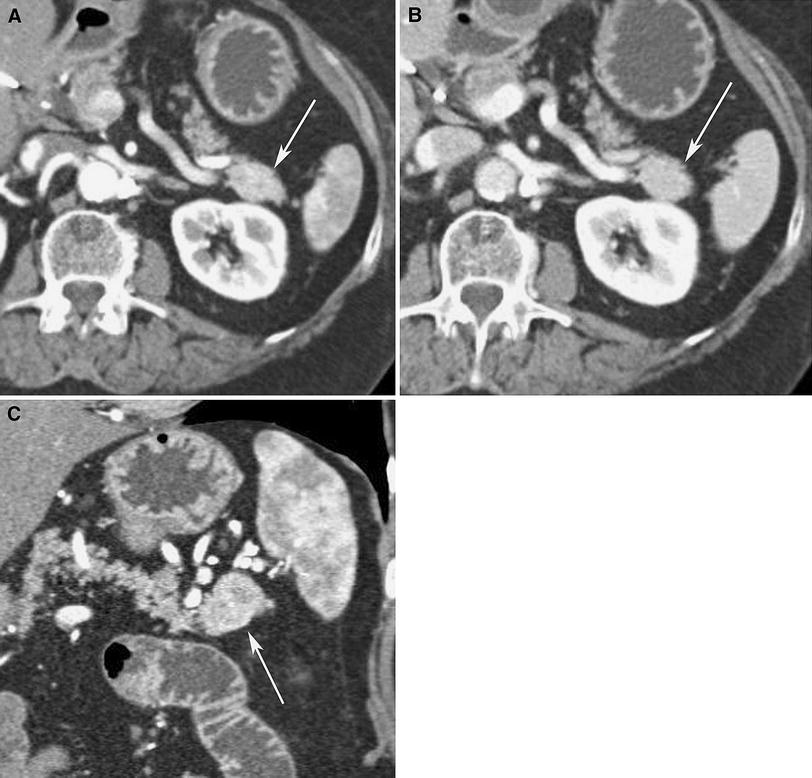
Fig. 5 81-Year-old woman with IPAS. Incidental mass in the tail of the pancreas was found by CT during evaluation of colonic diverticulitis. A Arterial and B portal venous phase axial CT images, and C arterial phase oblique coronal MPR image show 2.2 × 1.8 cm enhancing solid mass in the tip of the tail of pancreas (arrow). Note heterogeneous contrast enhancement within spleen and IPAS at arterial phase. Although IPAS was considered, nonfunctioning pancreatic neuroendocrine neoplasm could not be excluded, and patient underwent distal pancreatectomy and splenectomy. Pathology revealed IPAS.
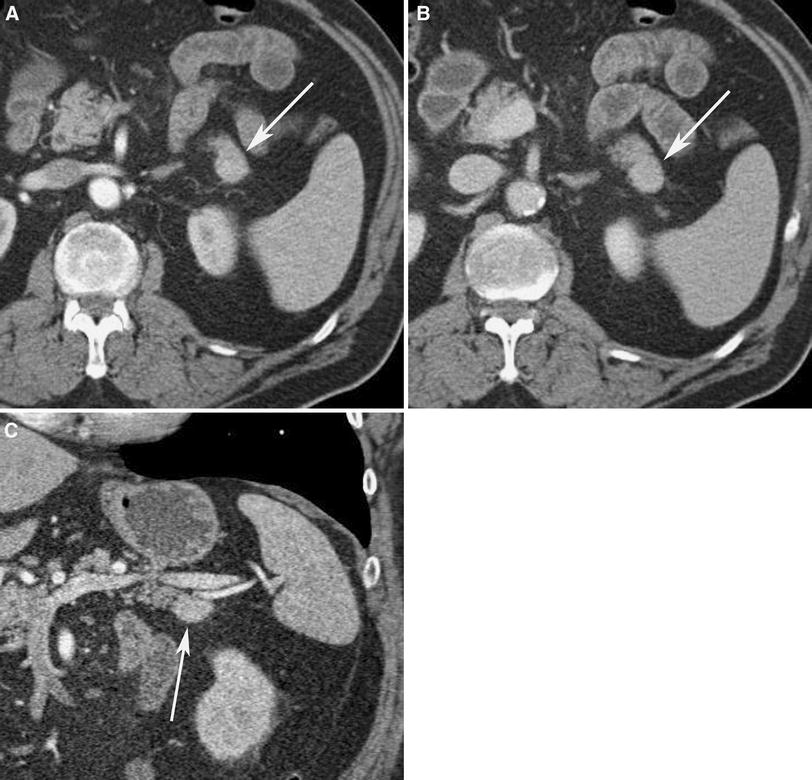
Fig. 6 75-Year-old man with mass in the tail of the pancreas incidentally found during evaluation for trauma. A Arterial and B portal venous phase axial CT images, and C arterial phase coronal MPR image show 2.4 × 2.5 cm enhancing solid mass (arrow) in the tip of the tail of the pancreas. Heterogeneous contrast enhancement pattern during arterial phase is not clear either in spleen or IPAS. Tc-99m sulfur colloid scintigraphy was negative. pancreatic neuroendocrine neoplasm was suspected, and patient underwent distal pancreatectomy and splenectomy. Pathology revealed IPAS.
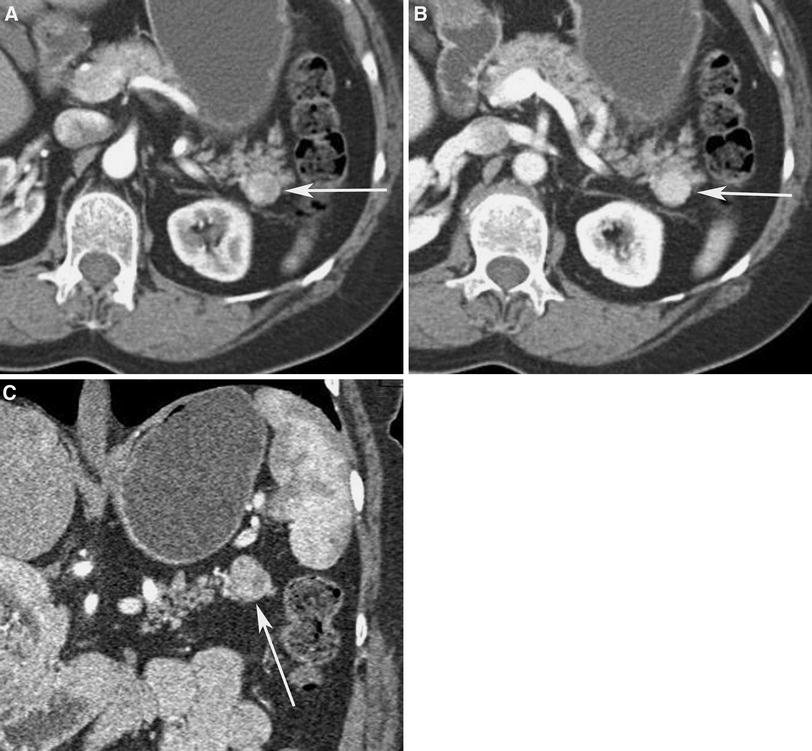
Fig. 7 60-Year-old man with incidentally found mass in the tail of the pancreas on chest CT. A Arterial and B portal venous phase axial CT, and C arterial phase oblique coronal MPR images show 1.8 × 1.8 cm enhancing solid mass (arrow) along dorsal aspect of the tail of the pancreas. Mass (arrow) is minimally lobulated and heterogeneously enhancing, similar to spleen during arterial phase. Although IPAS was considered, nonfunctioning pancreatic neuroendocrine neoplasm could not be excluded, and patient underwent distal pancreatectomy and splenectomy. Pathology revealed IPAS.
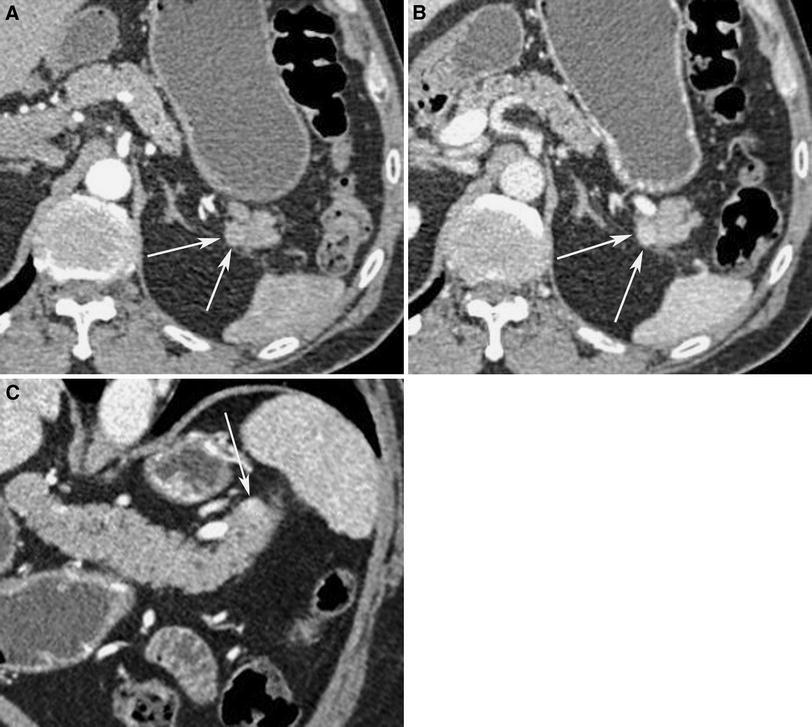
Fig. 8 72-Year-old man with incidentally found mass in the tail of the pancreas on a CT performed at another institution. A Arterial and B portal venous phase axial CT Images, and C portal venous phase oblique coronal MPR image show subtle 1.1 × 1.1 cm enhancing solid mass (arrow) along dorsal aspect of the tail of the pancreas. Mass (arrow) enhances similar to spleen. Although IPAS was considered, nonfunctioning pancreatic neuroendocrine neoplasm could not be excluded, and patient underwent distal pancreatectomy and splenectomy. Pathology revealed IPAS.
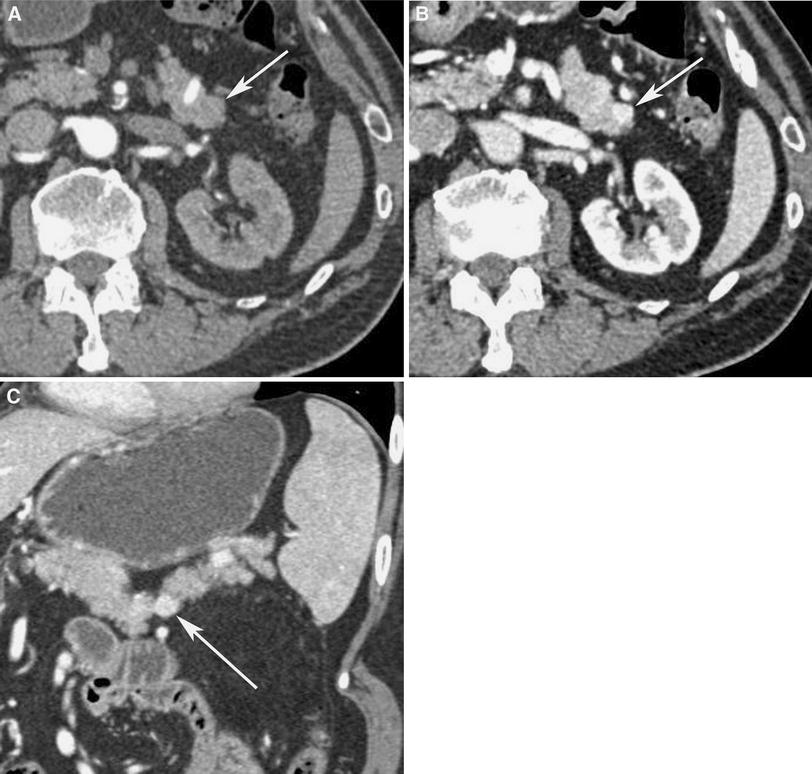
Fig. 9 68-Year-old man with incidentally identified small enhancing mass at the junction of the body and tail of the pancreas. A Arterial and B portal venous phase axial CT images, and C portal venous phase oblique coronal MPR image show subtle 1.2 × 1.0 cm enhancing solid mass (arrow) along the anterior aspect of the junction of body and tail of pancreas. Note mass enhanced greater than spleen on portal venous phase. Nonfunctioning pancreatic neuroendocrine neoplasm was suspected, and patient underwent distal pancreatectomy and splenectomy. Pathologically, this was well-differentiated pancreatic neuroendocrine neoplasm.
Halpert et al reported by autopsy data that 23 of 37 (62%) IPASs were partly embedded in the substance of the pancreas, whereas 14 (38%) were completely surrounded by the pancreatic tissue and their presence could be ascertained only on cur surfaces [8]. This autopsy study included 36 IPAS that ranged from 0.3–3.5 cm. In our experience, when IPAS is observed on CT, it is not often completely surrounded by the pancreatic parenchyma, and a part of the surface of IPAS is exposed to the peripancreatic fat (Figs. 2, 3, 4, 5, 6, 7, 8). IPASs that are completely surrounded by pancreas are likely small, but those small IPAS may not be visualized on CT.
Also in our cases, when an IPAS is located close to the tip of the tail of the pancreas, the exposed surface of IPAS (i.e., incompletely surrounded by the pancreatic tissue) is often seen along the dorsal surface of the pancreatic tail (Figs. 7, 8), than along the anterior surface of the pancreatic tail. However, further data are needed to confirm this finding.
CT attenuation and enhancement pattern
The blood supply to an accessory spleen is usually derived from the splenic artery, with drainage occurring into the splenic vein [11]. Accessory splenic tissue tends to exhibit the similar attenuation both on noncontrast and postcontrast scans, and same pattern of contrast enhancement as does the spleen itself on all phases [6, 12, 13].
Arterial phase CT imaging may be particularly helpful, especially when the characteristic heterogeneous, serpiginous enhancement pattern of normal spleen is also observed within IPAS (Figs. 2, 5, 7). This characteristic heterogeneous enhancement pattern is likely related to the unique histology of the vascular system of the spleen and the different flow rate through the cords of the red pulp and white pulp [6, 12]. It needs to be noted that heterogeneous enhancement pattern may not be detected or appreciated in IPAS at arterial phase CT (Figs. 6, 8) even when the main spleen has a serpiginous enhancement pattern [10], especially when the IPAS is small.
On venous phase CT imaging, IPAS also shows same pattern of contrast enhancement as does the spleen. Typically, IPAS enhances homogeneously and to the same degree as the spleen (Figs. 2, 3, 4, 5, 6, 7, 8). It follows that if the enhancement pattern of a mass within the tail of the pancreas is different from the spleen on either phase of contrast enhancement, it is unlikely to represent IPAS (Figs. 9, 10, 11, 12).
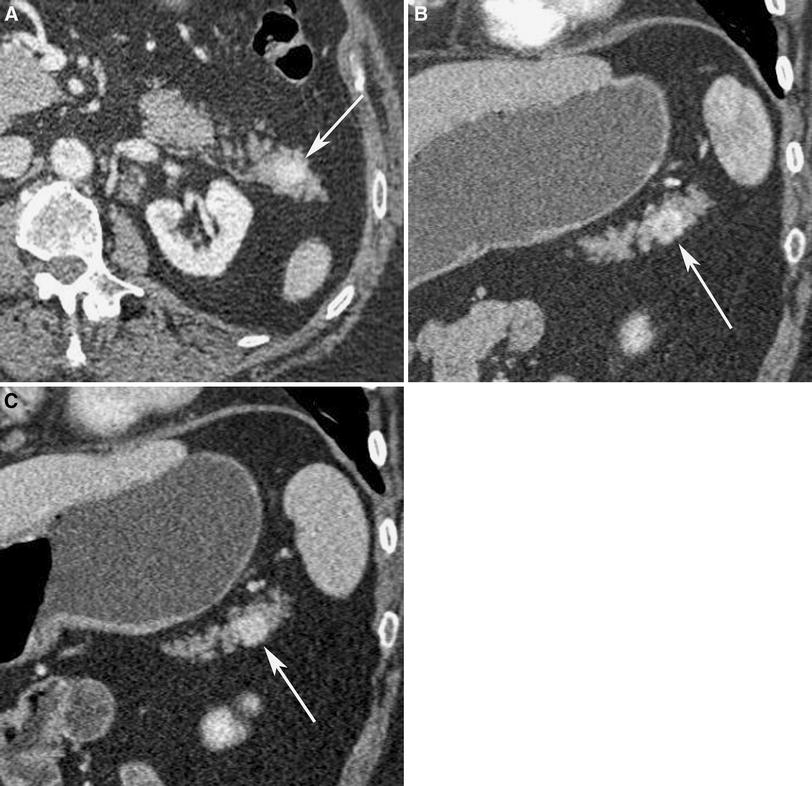
Fig. 10 58-Year-old woman with history of von Hippel-Lindau disease, status post bilateral adrenalectomies for pheochromocytomas. A Portal venous phase axial CT image, and B arterial and C portal venous phase oblique coronal MPR images show 1.7 × 1.5 cm enhancing solid mass in the tail of the pancreas. Note mass enhances greater than spleen during both arterial and portal venous phases, and shows ring-like enhancement at arterial phase (B). Patient underwent distal pancreatectomy and splenectomy. Pathologically, this was well-differentiated pancreatic neuroendocrine neoplasm.
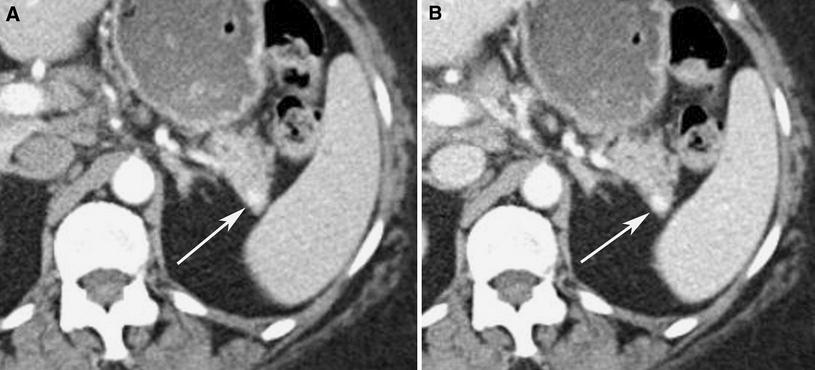
Fig. 11 61-Year-old woman imaged for evaluation of cirrhosis, disclosing unsuspected mass in the tail of the pancreas. A Arterial and B portal venous phase axial CT images show 0.8 cm enhancing solid mass in the tail of pancreas. Note that mass enhances greater than spleen at arterial and portal venous phases. Patient underwent distal pancreatectomy and splenectomy. Pathologically, this was well-differentiated pancreatic neuroendocrine neoplasm.
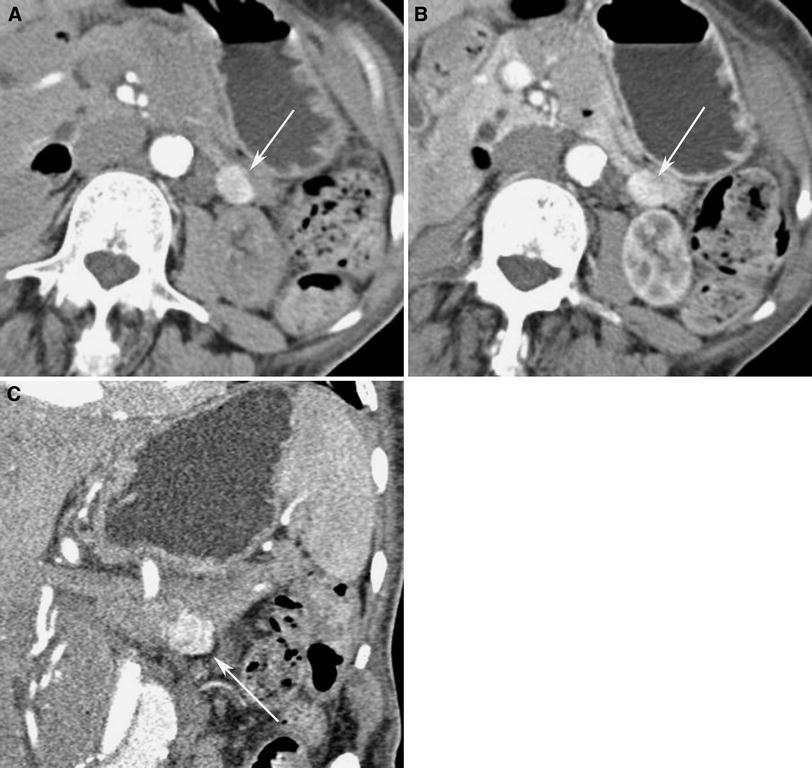
Fig. 12 83-Year-old woman with remote history of renal cell carcinoma, status post right nephrectomy more than 30 years ago. A Arterial and B portal venous phase axial CT images show enhancing solid mass (arrow) in the tail of the pancreas. C Arterial phase oblique coronal MPR image shows that mass (arrow) enhances greater than spleen at arterial phases. Fine needle aspiration under endoscopic ultrasound revealed metastatic renal cell carcinoma.
Differential diagnosis of IPAS
The most important differential diagnosis of IPAS is asymptomatic pancreatic neuroendocrine neoplasm. In review of surgically resected cases of IPAS, the most common preoperative diagnosis was nonfunctioning pancreatic neuroendocrine neoplasm [13]. Both IPASs and pancreatic neuroendocrine neoplasms are typically hyperenhancing on contrast enhanced CT (Figs. 9, 10, 11). Pancreatic neuroendocrine neoplasms are typically hypervascular, particularly on arterial phase, and may demonstrate uniform or ring-like enhancement [14] (Fig. 10). However, in some cases, pancreatic neuroendocrine neoplasms will be more enhancing on the venous phase acquisition (Figs. 9, 11). Furthermore, when the mass within the tail of the pancreas is small, the pattern of contrast enhancement may be difficult to analyze on CT (Fig. 11).
An alternative but uncommon differential diagnostic consideration is metastasis to the pancreas. Metastases from renal cell carcinomas often have a hypervascular appearance (Fig. 12), which can have an appearance similar to IPAS [15]. Clinical history of renal cell carcinoma helps to make the correct diagnosis.
An important pitfall to recognize is that nonneoplastic hypervascular lesions, such as splenic artery aneurysm, may simulate IPAS. In these cases, the enhancement pattern of aneurysm is identical to the vessels, and usually can be easily differentiated from IPAS, particularly when evaluated with 3D rendering to clearly demonstrate the relationship of aneurysm to the splenic artery (Fig. 13).
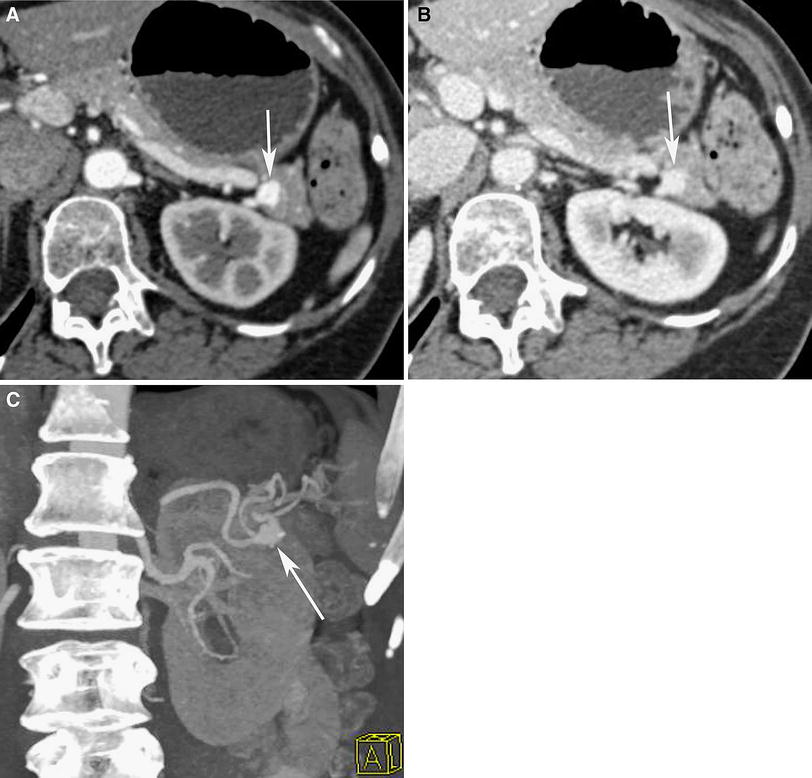
Fig. 13 67-Year-old woman imaged for evaluation of pancreatitis. A Arterial and B portal venous phase axial CT images show 1.0 cm vascular mass in the tail of the pancreas, which enhances similar degree to the abdominal aorta. C Oblique anterior MIP image confirms that this is 1 cm aneurysm arising from the splenic artery.
Correlative imaging
Technetium-99m (99mTc) labeled sulfur colloid or 99m Tc labeled heat-damaged red blood cell (HDRBC) scintigraphy has been used to diagnose ectopic splenic tissue (Fig 2). However, use of 99mTc labeled HDRBC scintigraphy is preferred because of reduced uptake by normal liver tissue resulting in improved target-to-background ratio [16] and higher sensitivity of 99mTc labeled HDRBC than 99mTc sulfur colloid scans to detect accessory spleen or splenosis [17, 18]. In reported cases and in our experience, IPASs that are less than 2 cm can result in false negative 99mTc sulfur colloid SPECT scintigraphy [19]. On the other hand, 99mTc labeled HDRBC scintigraphy is a highly specific method for detecting IPAS, as up to 90% of the injected HDRBCs are trapped by splenic tissue [20]. Nonetheless, when minimal functioning splenic tissue is present, or the lesion is small, visualization of IPAS may be still difficult due to inferior spatial resolution compared to other cross-sectional imaging modalities [6]. For example, Kim et al have reported a 1.1 cm IPAS that was missed on 99mTc labeled HDRBC SPECT scintigraphy [6].
There are a few reported cases of IPAS or splenosis in the pancreas, in which 111In somatostatin receptors scintigraphy (Octreoscan) was performed due to suspicion of pancreatic neuroendocrine neoplasm resulting in false positive results [9, 21–23]. The likely cause for these false positives is the presence of somatostatin receptors within the splenic tissue, which also can bind octreotide with high affinity [22].
Superparamagnetic iron oxide (SPIO)-enhanced MRI can also be used for the diagnosis of IPAS. With SPIO-enhanced MRI, IPAS has a signal drop similar to that of the spleen [6, 10, 24]. SPIOs are phagocytosed by the reticuloendothelial system (RES), and SPIO-enhanced MR imaging is reported to be an excellent alternative to 99mTc labeled HDRBC scintigraphy for confirming the diagnosis of IPAS because of its higher spatial resolution than scintigraphy [5].
Reports describe the use of contrast-enhanced sonography, with a microbubble contrast agent, to reveal the characteristic enhancement feature of IPAS and allows the specific diagnosis of IPAS [3, 25]. Kim et al. observed six patients with IPAS who showed inhomogeneous enhancement in the early vascular phase, and prolonged enhancement in the hepatosplenic parenchymal phase (3–5 min after contrast injection) on contrast enhanced sonography, using galactose and palmic acid (Levovist; Schering, Germany) [25]. This agent is exclusively accumulated by the hepatic and splenic parenchyma due to RES activity on the delayed phase [3, 25].
Epidermoid cyst within IPAS
Epidermoid cysts, lined with squamous epithelium, can rarely occur within IPAS (Fig. 14). In these cases, the epidermoid cyst in the IPAS mimics a cystic neoplasm of the pancreas, often diagnosed as mucinous cystic neoplasm on imaging [26]. Motosugi et al. analyzed imaging findings of six such cases and reviewed 27 cases in the literature. They reported that the mean size of this cystic lesion was 3.7 cm, and 21 cases were unilocular (Fig. 14), and 13 cases were multilocular [26]. In 18 of 33 cases, normal splenic tissue surrounding the cyst, either mass-like or rim-like, was visible on radiological imaging or macroscopic photography [26]. This solid portion shows similar contrast enhancement pattern to the spleen on CT (Fig 14) or MRI, and it may be helpful for diagnosing this rare anomalous condition [6, 27].
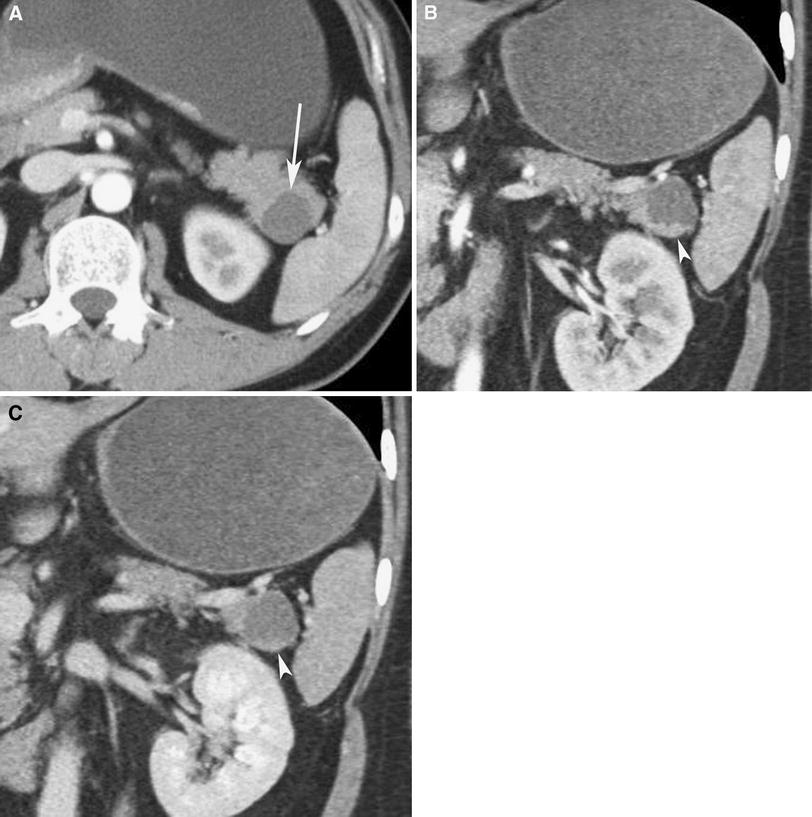
Fig. 14 41-Year-old woman who underwent CT for vague epigastric pain. A Arterial phase axial CT, and B arterial and C portal venous phase coronal MPR images show 2.4 × 2.3 cm cystic lesion in the tail of the pancreas with peripheral rim-like solid component that enhances similar to the spleen (arrowhead). Endoscopic ultrasound demonstrated mural nodularity. Tc-99m HDRBC scan performed at outside institution was reported to be negative. Patient underwent distal pancreatectomy and splenectomy. Pathologically, this was epidermoid cyst in IPAS.
Conclusion
In conclusion, IPAS should be considered when a hypervascular mass is seen in the tail of the pancreas. Radiologist should recognize the imaging overlap with hypervascular masses in the tail of the pancreas, particularly asymptomatic pancreatic neuroendocrine neoplasms. Typical location, similar attenuation of the lesion to the spleen on noncontrast, and postcontrast CT at different phases are helpful to make diagnosis of IPAS. In particular, characteristic heterogeneous contrast enhancement of IPAS during the early postcontrast phase may prove most helpful for correct diagnosis. However, when it remains difficult to exclude the other diagnosis, 99mTc labeled HDRBC scintigraphy or SPIO-enhanced MR imaging can be used to confirm the diagnosis of IPAS, with the caveats described above. Future research should be aimed at systematically comparing the CT appearance of IPAS and pancreatic neuroendocrine neoplasm, in terms of location within the pancreatic tail, percentage of exposure to the peripancreatic fat and enhancement relative to both pancreas and spleen, in an attempt to define reliable criteria for preoperative diagnosis.
References
